Karaganda State Medical University
Choices are denoted Excellent (E) / Good (G) / Poor (P)
Case 1. Askar Yusupov (Diarrhea)
Author: Dyssembayeva Ainash, Alshynbekova Gulsharbat
Case outline
Your patient is a 58 year old man, Askar Yusupov. He fell ill with fever to 39.30C, general weakness, severe headache, dizziness, nausea, urges to vomit, anorexy, abdominal pain, a feeling of "transfusion" in the intestines.He is ill the 1st day.
From the anamnesis of life:
He irregularly eats in the cafeteria of the college, is under regular medical check-up of a gastroenterologist for chronic gastritis from the age of 13. During the last 7 years, he is troubled by constipation, sometimes replaced by diarrhea. Askar smokes from the 13age.
On examination: Pulse - 88/min; Breathing rate - 26/min; Temperature – 39,30 C; Arterial blood pressure – 110 and 70mm. hg.art.
His appetite is absent. Skin is pale, there is no rash. Shadows are under his eyes. There is no thirst. In the oropharynx is slight hyperemia, tonsils are up to II size, there is no pus. The tongue is coated with a white coating, moist. The abdomen is rounded, slightly distended, increased bowel sounds. There is the pain in palpation of the abdomen in the epigastric and left ileac regions. The stool was this morning.
Choice 1 Treat in an outpatient department, general blood test (GBT), general urine test (GUT), coproscopy, bacteriological test of stool (E) / Ultrasound of the gastroduodenal zone, biochemical blood test, consultation of a gastroenterologist (P) / Admission in an infectious hospital (G)
Askar came to you for a reexamination, because he noticed a blood in the stool. His temperature is 37.50 C. He began to worry about cramping pain in the epigastric region and in the left ileac area, which begin before the act of defecation pass and after it. Yesterday, there was a 2-times per day vomiting after eating and fluid intake. Today there was no vomiting. Appetite is absent. He has weakness, headache.
On examination: His abdomen is soft, sunken, have a growling stomach, painful in the epigastric region and the left ileac region. Sigma is painful and dense. The liver and spleen are not enlarged. Diuresis is normal.
Choice 2 Consultation of an oncologist, digital rectal examination, sigmoidoscopy (G) / Treat in an outpatient department with antibiotic (E) / Consultation of the surgeon (P)
You explains him that from the results of the analysis it follows that he has inflammatory changes in the GBT; in GUT are no specific findings, in the coproscopy are inflammatory changes (hemorrhagic colitis), which can be a sign of dysentery. This fact is manifested by inflammation in the large intestine, and ulcers can form and as a consequence - blood in the stool.
Choice 3 Reexamination (E).
Askar came to you for reexamination. He is ill the 5th day. Temperature is normal.
It continues to worry him the pain in the epigastric region and cramping pain in the left ileac region, which begin before the act of defecation and pass after it. There is no vomiting. Appetite is absent. He has weakness, headache.
On examination: His skin is pale, dry, no rash. Shadows are on his skin under the eyes. There is no thirst. The tongue is coated with a white coating, dryish, salivation is reduced. The abdomen is rounded, distended, increased bowel sounds, painful in the epigastric region and the left ileac region. Sigma is palpated like a dense, painful. The liver and spleen are not enlarged. Diuresis is normal. Before the act of defecation, there is a dragging, spastic pain in the anus, accompanied by an urge to act of defecation and urination. Stool is up to 15 times a day.
He tooks aspirin and sometimes drotaverin only. S. Flexneri was found in the bacteriological test.
Anus is gaping. Mucous around the anus is hyperemic, macerated, from the anus extracted is bloody - mucous discharge in an insignificant amount. You notice the prolapse of the rectal mucosa.
Choice 4 Rectum rectification alone (P) / Surgeon consultation (E)
You ask the surgeon's doctor to consult Askar, in connection with the presence of prolapse of the rectal mucosa during the act of defecation.
On examination: In Askar, before the act of defecation, the dragging, spastic pain in the anus is preserved, accompanied by an urge to act of defecation and urination. The stool up to 15 times a day is poor, with a lot of mucus, greens and streaks of blood.
Anus is gaping. Mucous around the anus is hyperemic, macerated, bloody - mucous discharge in an insignificant amount is extracted from the anus. The prolapse of the rectal mucosa is noted.
The surgeon suggests that Askar set the rectal mucosa.
Choice 5 Continue an outpatient appointment with an doctor GP (E)
After consulting the surgeon, Askar again comes to you.
You explain to Askar that he cannot sit on the toilet for a long time during the act of defecation, and also say that it is necessary to continue taking drotaverin at 40 mg x t.i.d. for 3-4 days and with repeated prolapse of rectal mucosa. It is necessary again consult a doctor to correct it. If the recovery of mucosal prolapse of the rectum remains, then it will be necessary to perform surgical treatment.
Since it was output - S. Flexneri in bacteriological test, then necessarily treatment with an antibiotic - ciprofloxacin is necessary; without taking an antibiotic recovery is almost impossible and there can be an even greater deterioration in his condition.
Choice 6 Continue ambulatory treatment (E)
In the corridor of the clinic you see Askar. He came to you for a follow-up inspection. He is ill on the 10th day. Askar is dissatisfied, because he was tired of spending most of his time in the waiting list for consultants. You explain to Askar that you were forced to do this, because he needed their advice and, if necessary, corrected his treatment.
You ask permission to continue your inspection with Askar. Temperature on normal figures. Pain in his stomach does not bother him. Vomiting is not. Appetite appeared, and my mood improved. He has a slight weakness. The abdomen is rounded, painless when palpated, sigma is palpated in the form of a loose, painless crotch. Diuresis is normal. Stool up to 1-2 times a day.You evaluate the results of the coprogram after the treatment received.
Choice 7 To finish the course of antibiotic, with the subsequent discharge of the patient with registration of the documentation with recommendations (E) / Continue antibiotic treatment for 3 days, control copyscopy followed by patient discharge and documentation preparation with recommendations (P)
You decide to complete the antibiotic
You decide to finish the course of antibiotic, tk. there are no symptoms of intoxication, symptoms of a colitis syndrome. Stool - without pathological impurities. The results of the coprogram are easy enzymatic changes.
You tell this to Askar.
You warn him that he will be able to continue his education in college after passing the control pot of sowing feces, which must be taken 2 days after antibiotic therapy.
In addition, you recommend him a gradual expansion of the diet, taking a biopreparation, enzymes for 2 weeks.
Askar thanks you and leaves.
Learning Objectives:
- Ethiology, epidemiology,
- pathogenesis of shigellosis,
- clinical presentation and differential diagnosis of shigellosis andmucosal prolapse of rectum, rational therapy of shigellosis.
Errors covered:
- Insufficient skills,
- Poor communications,
- Playing the odds,
- Bravado
Case 2. Nurbol Asanov (Dyspnea)
Author: Aizhan Beisenaeva, Ainash Ibysheva
Case outline
You are a second-year intern, you are admitted to the clinic as a GP. You have a patient at the reception: Asanov Nurbol, 18 years old. According to Nurbol, he called a doctor at home 4 days ago about raising the temperature to 38 ° C, rhinitis, sore throat and painful dry cough. These symptoms disturbed Nurbol for 6 days. The doctor then prescribed paracetamol, ambrobene, recommended irrigation of the throat with furacilin solution. On the third day, the temperature returned to normal, but the cough grew steadily, especially disturbed at night and in the early morning hours.
Such a cough disturbed Nurbol even earlier, with every ARVI and ARD, but in the last 1-1.5 years it's worried without the cold, during physical activity (running, jumping, outdoor games), laughing; Also, sometimes Nurbol wakes up at night from the feeling of lack of air and coughs heavily, this happens on average 2 times a week.
From the anamnesis of life:
In childhood, Nurbol often suffered from acute respiratory viral infections, which developed into bronchitis and pneumonia. Over the past 12 months, Nurbol suffered acute respiratory diseases 5 times, self-took amoxicillin.
Allergic history: allergic to penicillin and honey, manifested by urticaria. Heredity: the mother suffers from high artery pressure, has a heart disease. Nurbol knows nothing about his father’s diseases, but notes that his father has been smoking for 10 years.
On examination: Increased nutrition. Height is 165 cm. Weight is 95 kg. Body temperature 36.6 ° C
Pale skin. Breathing through the nose is difficult. The mucosa of the posterior pharyngeal wall is slightly hyperemic. Thorax regular shape. BR 25. In the lungs vesicular breathing, slight wheezing in all the pulmonary fields are heard. Heart sounds are clear, correct rhythm. HR 95 b/min. Pulse 95. Artery pressure 120/80 mm.rt.st on both hands. Abdomen with palpation is soft, painless. Liver at the edge of the costal arch.
Choice 1 Send for general blood analysis, spirometry, bronchodilator test (E) / Send to GBA, ECG, Echo-CS (P) / Send to chest X-ray, GBA, BС of blood (G)
The next day, Nurbol Asanov came to your reception. You evaluate the results of research already obtained.
Choice 2 Assign inhalation salbutamol at coughing attacks (G) / Refer to an allergist (E) /
An allergist has studied in detail the data of anamnesis and studies conducted in the clinic. The doctor prescribed tests to clarify the allergic status of Nurbol - ELISA for JgA and allergy tests. The diagnosis of Nurbol in the clinic was confirmed by a GP doctor. An allergist prescribed a second stage of treatment of bronchial asthma according to the Gina program, recommended avoiding hypothermia of provoking factors, a hypoallergenic diet. You are a second-year intern, substitute at the reception of the therapist who is on vacation. You have a patient Nurbol 18 years old at the reception, he came for a prescription for drugs on the GFMС. He was consulted by an allergist four weeks ago, he was diagnosed with bronchial asthma. As prescribed by the allergist, he takes beclamethasone 200mg inhalation 1 time per day, salbutamol through an inhaler on demand and before physical exertion. Nurbol told you that he uses Beklamethasone inhalation 1 time a day in the morning, salbutamol inhalation 1 time before football training, and also when he wakes up at night from feeling short of breath and difficulty in breathing (about 1 time a week).
Objectively: The skin is clean, pink. On the hyperemic mucous membrane of the oral cavity a cheesy patina, film is visible; plaque loosely lies on the underlying tissues, is easily removed, while not damaging the mucous membrane, which retains a smooth, smooth surface and red color; Thorax regular shape. BR 18. Vesicular breathing in the lungs, no wheezing. Heart sounds are clear, rhythmic. HR 75 beats / min. AP 120/80 mm.rt.st. The abdomen is soft, painless.
Choice 3 Increase IGCS dose to medium, recommend mouth rinsing after each IGCS application (P) / Increase IGCS dose to medium, recommend using inhaler activated by inhalation (DAI-BA) (G) / Leave low dose IGCS, recommend using inhalers with spacer (E).
Learning Objectives:
- Ethiology, pathogenesis of bronchial asthma,
- Clinical presentation and differential diagnosis of bronchial asthma,
- Rational therapy of bronchial asthma.
Errors covered:
- Ignorance,
- Bravado,
- Insufficient skills
Case 3. Marzhan Akhmetova (acute abdomen)
Case outline
You are an intern / resident general practitioner in the city polyclinic №3. Your next patient is Marzhan, 17 years old. On January 6, 2017, her grandmother brought you a checkup to make sure everything was in order.
Marzhan complained of a rise in temperature of up to 37 ° C, headache, fatigue, fatigue, loss of appetite.
From the anamnesis of life:
Heredity is not burdened. From past diseases: acute respiratory diseases, chicken pox in 3 years old.
She lives with his grandmother, because his mother is constantly on business trips. In the history of the words of her grandmother, she and her mother went to a gastroenterologist.
Tuberculosis, viral hepatitis, sexually transmitted diseases denies.
Allergic history is not burdened.
Family history is not burdened.
Bad habits denies.
Nutrition full, regular.
On examination: Marzhan is pale, blue under the eyes. Calm, shy, polite, smiling. Studying well.
When asked about her symptoms, she respond with medical terms from the Internet.
The tongue is thickly coated with white bloom, palms are wet.
Heart sounds are deaf, arterial pressure is 100/60 mm.rt.st. HR - 83 beats in min
On examination, the abdomen is slightly swollen and tense. There is pain with deep palpation more to the right.
Symptom tapping negative.
Choice 1 Send for consultation to the gynecologist (E) / Determine the level of human chorionic gonadotropin in the blood and urine (G) / Make culdocentesis (E)
Considering complaints about fever up to 37.2 С0, headache, fatigue, loss of appetite, taste perversion, nausea, single vomiting in the mornings during the last week, aching pain in the lower abdomen, which is replaced by periods of cramping pain and short periods well-being. Gynecological history: menarche from 14 years, the menstrual cycle is not established, for 5 days after 28-32 days. The menstrual cycle is irregular, menstrual periods are moderate, sometimes accompanied by painful sensations on the first day. Lives sexually since 16 years. The last menstruation is December 18-20 (Marzhan cannot give an exact date). Objective examination: the tongue is thickly coated with white bloom, palms are wet. Pallor of the skin and mucous membranes. Heart sounds are deaf, arterial pressure is 80/60 mm.rt.st. HR - 96 beats per minute, weak filling of the pulse. When examining the mammary glands: the mammary glands are round, with palpation sensitive, swollen, there is a release of colostrum when pressed on the nipples. The abdomen is somewhat swollen, soft, painful on palpation in the lower sections, more to the right. For gynecological examination in the mirrors: Cyanosis of the vaginal entrance, the mucous membrane of the vagina and cervix. When bimanual examination: The uterus is enlarged and softened. In the area of the uterine appendages on the right side, a tumor-like formation of a testovaty consistency is palpated, painful in the study. Per rectum: in the uterine rectangular space, smoothness or bulging of the posterior vaginal fornix, markedly painful on palpation, is noted. On pelvic ultrasound, an increase in the body of the uterus, a thickening of the endometrium, the ovum is absent, fluid accumulation in the dorsal space (blood), a heterogeneous formation with fuzzy contours in the projection of the uterus appendages.
You are not wasting time determine the level of HCG in the urine, doing culdocentez. During the puncture of the posterior fornix, aspirate free blood and send Marzhan to the gynecological department for hospitalization, for surgical intervention with removal of the ectopic pregnancy in the fallopian tube.
In the postoperative period, you give recommendations on the use of modern methods of contraception (COC) for 6 months, for planning pregnancy.
Choice 2 Give directions to GBA, GUA, Gastroscopy, abdominal ultrasound (P) / Assign paracetamol, antibiotic, follow-up appointments in 3 days (P) / Determine the level of human chorionic gonadotropin in the blood and urine (G) / Make culdocentesis (E) / / Send for consultation to the gynecologist (E)
Choice 3 Send for consultation to the surgeon (G) / Determine the level of human chorionic gonadotropin in the blood and urine (G) / Send for a consultation to the gynecologist (E) / Make a culdocentesis (E)
Learning Objectives:
- The concept of "extrauterine pregnancy"
- Diagnostic criteria of extrauterine pregnancy according CP
- Differential diagnosis of the syndrome of "Acute abdomen"
- Tactics of management of patients with syndrome "Acute Abdomen"
- Tactics of management of women with extrauterine pregnancy in the postoperative period
- Preventive measures: timely and correct tactics of patient management during the first treatment; timely diagnosis and treatment of infectious and inflammatory diseases of the pelvic organs; abortion prevention; use of modern contraceptives.
- Further management: the use of modern methods of contraception (COC) for 6 months; pregnancy planning advice.
Errors covered:
- Lack of knowledge
- Bravado
- Fixing
- Bad teamwork
- Lack of skills.
Case 4. Victoria Lavrova (Intoxication)
Author: Aizhan Beisenaeva, Ainash Ibysheva
Case outline
You are a doctor of general practitioner, Victoria Lavrova came to you, she is 24 years old. Victoria told you that for 1.5 months she was worried about weakness and fatigue, in the last 2 weeks her body temperature rose to 37.7 ° C.
From the anamnesis of life:
Independently took paracetamol. She asks you to write her a prescription for iron and vitamins, since She believes that she has anemia or hypovitaminosis, because 2 months ago she gave birth to a child and is now feeding with breast milk.
She noted a certain stiffness in the mornings in these joints; she connects this with contact with cold water, since often have to be washed by hand. Victoria is also studying to be a hairdresser, she has to load her hands during practice.
On examination: Decreased appetite. Weight - 52 kg. Height - 164 cm. The skin and visible mucous pale. Bone system without visible deformations. Visually determined slight swelling of the proximal interphalangeal joints of 2-3 fingers on both hands. Muscle strength is normal. Symptom compression of the brush is positive. Submandibular and cervical lymph nodes with a diameter of up to 0.5 cm are palpable. Heart sounds are clear, the rhythm is correct. HR - 92 per minute. AP - 110/70 mm.rt.st. In the lungs vesicular breathing, wheezing is not heard. RR - 18 per minute. The abdomen of the usual form, palpation is soft, painful in the epigastric region. The liver does not protrude from the edge of the costal arch; Kurlov sizes: 10x8x7 cm. Spleen not palpable; percussion its dimensions: 10.5x5 cm. The chair is dark brown in color, decorated. There are no dysuric phenomena. Symptom tapping negative on both sides. Peripheral edema no.
Choice 1 Examine the patient (E) / Assign iron supplements and calcium supplements (P) / Assign iron supplements, diclofenac ointment, limit contact with cold water (G)
You wrote out directions for an immunoassay for STDs (chlamydia), immunological tests for the determination of antinuclear antibodies and antiphospholipid antibodies, also a test for determining the ACCP, Wright-Heddelson's reaction, explained to Victoria that you suspect a number of diseases of the joints, and you need to further examine her.
Choice 2 Assign a test for determining ANA, ANF and ACCP (E) / Assign a test for determining ANA, APA and LIA for chlamydia (P) / Assign LIA for chlamydia and test for ACCP (G)
You- the GP, at the reception of the patient Lavrova Victoria, look at the results of the analyzes.
ACCP - negative.
Immunology test: ANA titer below measuring range (negative), APA titer below measuring range (negative)
Choice 3 Assign diclofenac i/m, ointment ketorol locally (P) / Hospitalize as planned (G) / Rheumatologist's consultation (E).
You are a rheumatologist. Patient Lavrova Victoria, 24 years old has been sent to you for a consultation. Victoria sent you a GP with a diagnosis of unspecified arthritis.
You decide to examine her: Bone system without visible deformations. Visually determined slight swelling of the proximal interphalangeal joints of 2-5 fingers on both hands. Muscle strength is normal. Symptom compression of the brush is positive.
Choice 4 Assign methotrexate + diclofenac (E) / Assign prednisolone (P) / Assign Sulfasalazine + diclofenac (G)
Learning Objectives:
- Ethiology, pathogenesis of rheumatoid arthritis,
- Clinical presentation and differential diagnosis of rheumatoid arthritis,
- Rational therapy of rheumatoid arthritis,
- Features of conducting patients with rheumatoid arthritis.
Errors covered:
- Ignorance,
- Insufficient skills,
- System error,
- Bravado,
- Timidity
Case 5. Ermek Kunaev (abdominal pain)
Author: Dobler K.E., Amangeldiyeva K.K.
The first patient: Ermek Kunaev, a 53-year-old man with severe epigastric pain, nausea, vomiting, and occasional belching with air.
The second patient: Maryam Ilyasova, a 48-year-old woman with severe pain in the lumbar region on the right, with frequent urination.
The third patient: Oleg Samsonov, a 49-year-old man with fever up to 39 ° C, a wet cough, shortness of breath (RR 32 per minute).
Who do you think which patients should be examined first
Choice 1 E first patient
Choice 2 P second patient
Choice 3 P third patient
Case outline
In the clinic
You have begun inspection of Ermek Kunaev. A 53-year-old man with severe pain in the epigastric region, nausea, vomiting, and occasional belching with air.
From the anamnesis of life:
From the anamnesis, we learned that these complaints (pains in the epigastric region, nausea, vomiting, periodic belching with air) began to bother the patient in the last 2 hours after emotional overstrain (quarreled with his son), appeared suddenly. Independently, I took omeprozole 1 capsule 20 mg and cerukal 1 tablet 10 mg. The state after this has not improved.
On examination: The skin is pale, moist, with cold sticky sweat, there is a slight cyanosis of the lips, the face expresses anxiety.
Respiratory system: RR-27 per minute, vesicular breathing in the lungs, no wheezing.
Cardiovascular system: HR-102 per minute, marked rhythm disturbance. Borders of the heart are expanded, deaf tones. AP 100/65 mm.rt.st.
Gastrointestinal tract: Tongue clean, moist. On palpation of the abdomen, pain is noted in the epigastric region, muscle tension in the abdominal wall, abdominal distention and participation in the act of breathing are also noted. Chair unchanged 1 time per day. Urination free, painless.
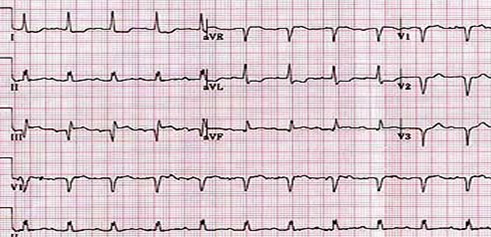
To the patient at your insistence was made an ECG.
Your next steps:
Choice 1 Assigning GBA, BCA of blood to myocardial necrosis markers and total B/c blood CITO (E)
Choice of 1a i/v aspirine, morphine and hospitalization in the therapeutic department (E)
Choice of 1b to appoint nitroglycerin 1t sublingually, aspirin 1t, furosemide iv, lower the legs below the level of the body (P)
On the basis of laboratory tests and an ECG, made in the emergency room by a doctor of a therapeutic department, a diagnosis of acute intramural myocardial infarction was made.
Choice 1a. After the introduction of morphine and aspirin, Ermek's condition improved. Ermek will be hospitalized for 14 days.
Choice 1b The patient's condition worsens and enters the intensive care unit.
Choice 2 Give the patient a referral to an ultrasound scan of hepatoduodenal area, gastroscopy and consultation to a gastroenterologist (G)
Choice 2а i/v aspirine, morphine and hospitalization in the therapeutic department. Assigning GBA, BCA of blood to myocardial necrosis markers (G)
Choice 2b Assign nitroglycerin 1t, sublingually, digoxin 0.25 1 time per day, Veroshpiron 100mg 2 times per day (P)
Choice 2c Assign nitroglycerin 1t sublingually, aspirin 1t, furosemide iv, lower the legs below the level of the body (P)
At the reception at the gastroenterologist, the condition of Ermek was close to severe .. Ermek Kunaev was urgently hospitalized in serious condition in the intensive care unit. A cardiologist was called to the intensive care unit for a consultation. He looked at an ECG made earlier and examined the patient. An ECG given an intramural IM conclusion.
Choice 2a After all the laboratory and instrumental examinations, the doctor of the cardilogue was very distressed that the patient with acute myocardial infarction was not hospitalized in a timely manner and was not prescribed the necessary assistance.
Choice 2b. Choice 2c. After 30 minutes the patient's condition worsened. RR 38 per minute, single pulse, AP 50/30 mm.rt.st The patient was urgently transferred to the intensive care unit. Physicians in intensive care for 30 minutes took resuscitation measures in an attempt to save the patient, including febrillation, but all of them turned out to be ineffective. The patient died.
Choice 3 Hospitalization of the gastroenterology department with the appointment of ultrasound scan of hepatoduodenal area, gastroscopy, GBA, BCA of blood (G)
Learning Objectives:
- Ethiology,
- pathogenesis of myocardial infarction,
- Clinical presentation and differential diagnosis of myocardial infarction,
- Rational therapy of myocardial infarction,
- Features of conducting patients with myocardial infarction.
Errors covered:
- Sort Error.
- Fixation.
- Lack of knowledge.
- A game in the odds.
- Negligence.
Case 6. Bleeding (Serik Nurzhanov)
Case outline
You are a general practitioner intern. At the reception, the patient Nurzhanov Serik, 40 years old. She complains of weakness, palpitations, dizziness, headaches, tinnitus, shortness of breath on exertion, cough with poor sputum, abdominal pain, vomiting in the morning due to strong cough, dark brown vomiting mass, rusty.
From the anamnesis of life:
A history of chronic bronchitis, chronic gastritis, chronic cholecystitis. Often takes painkillers. Mother has arterial hypertension, father died of stomach cancer.
On examination: The patient is very restless. The state of moderate severity. Body temperature - 37.4 ° C. Asthenic physique. The skin and visible mucous pale pink, no rash. Peripheral lymph nodes are not enlarged. Chest emphysematous, at palpation elastic.
In the lungs breathing hard, no wheezing. BR-19 per minute. Heart tones are muffled, at the top of the systolic murmur, the rhythm is not correct. HR-90 beats per minute. AP - 100/70 mm Hg. The tongue is coated with white bloom. On palpation, the abdomen is slightly painful in the epigastric region. Symptoms of peritoneal irritation no. Liver, spleen not enlarged. Diuresis is normal. The chair is prone to constipation.
Choice 1 (E) Assign GBA, Esophagogastroduodenoscopy, surgeon consultation, emergency hospitalization.
The next day, Nurbol Asanov came to your reception. You evaluate the results of research already obtained.
Body temperature - 37.4 ° C. The skin and visible mucous pale pink, no rash. Cold sweat. In the lungs breathing hard, no wheezing. BR-19 per minute. Heart tones are muffled, at the top of the systolic murmur, the rhythm is not correct. HR-91 beats per minute. AP- 90 / 60mm.rt.st. The tongue is coated with white bloom. Abdomen palpation more painful in the epigastric region. Symptoms of peritoneal irritation no. Diuresis is normal. The chair wasn't more than 3 days.
Choice 2 (G)
Chest X-ray, sputum analysis, Assign GBA, GUA, biochemical blood test, Treat at the site with drugs Ғe and control examination after 1 month.
Serik came to re-reception. All complaints are saved. Body temperature - 37.5 C. Complaints of severe weakness, palpitations, dizziness, headaches, shortness of breath on exertion, cough with sputum secretion persist. He is very restless. Last night there was rusty vomiting after eating.
Choice 3 (P)
Oncologist's consultation, Assign GBA, GUA, biochemical blood test, Esophagogastroduodenoscopy, surgeon consultation, Gastroenterologist consultation
You recommend Serik to sign up for a gastroenterologist tomorrow, explaining that this specialist is competent in this disease much better than a general practitioner.
At night, Serik's condition worsened. The wife called an ambulance. Upon arrival of the emergency doctor: the patient is adynamic, inhibited, systolic blood pressure below 70 mm.rt.st., pulse more than 120 in 1 minute, filamentous, CVP is 0 or negative, there is a lack of urine (anuria). Serik in a serious condition was immediately hospitalized.
A history of hemoptysis can lead a doctor to suspect cancer, considering the factor that the father of the patient died from it, plus the presence of an appropriate history. This leads to the fact that the patient did not have needed help, and even though the conducted research and consultations with young doctor can question the decision of a correct diagnosis, thus the patient may lose a lot of blood and even conducted emergency activities to be fatal.
Learning Objectives:
- Ethiology, pathogenesis of bronchial asthma,
- Clinical presentation and differential diagnosis of Bleeding stomach ulcer ,
- Rational therapy of Bleeding stomach ulcer.
Errors covered:
- Lack of knowledge.
- System error.
- Negligence.